The contents of this article include:
1) What is cervical cancer? Who gets cervical cancer?
2) Causes and early signs of cervical cancer?
3) How to prevent cancer of the cervix
4) FIGO stages of cervical cancer
5) Treatment options for cancer of the cervix?
6) Best cervical cancer treatment hospitals
Cervical Cancer Causes | Stages | Best Treatment Hospitals
Did you know the World Health Organisation aims to eliminate cervical cancer by 2030?
With early detection through regular screenings like Pap smears and HPV testing, cervical cancer can be largely prevented.
Early detection allows for more successful and less invasive treatment options, significantly improving the chances of a full recovery.
Cervical cancer is the fourth most common cancer among women, with an estimated 660,000 diagnoses of new cases globally annually.

In this article, we'll shed light on the causes and stages of cervical cancer. We'll explore the latest treatment options, such as proton therapy in India, chemotherapy and radiation.
For those seeking the best possible care, we'll unveil a network of the best cancer treatment hospitals, ready to support you on your journey to recovery.
Get connected to some of the Best Cervical Cancer Specialists for FREE!
What is Cervical Cancer
Cervical cancer occurs when cells of the cervix (the opening of the uterus) change first by becoming pre-cancerous, then cancerous, forming growths on the exterior of the cervix.
Who Gets Cervical Cancer?
It is often diagnosed in young to middle-aged women, with many of them being 35 to 44 years old.

However, recently more than a third of new diagnoses have been found to be in women between 20 – 44 years old.
What Are the Causes of Cervical Cancer?
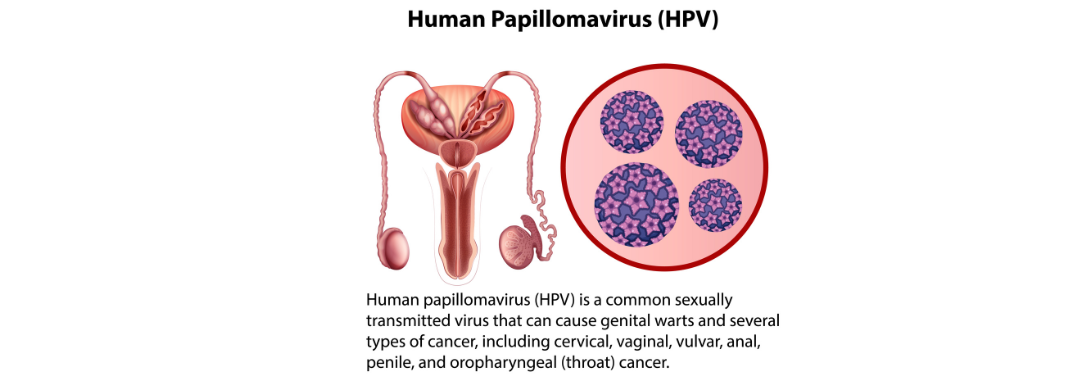
1) HPV (Human Papillomavirus) causes nearly 90% of cervical cancers, spread through skin-to-skin contact, particularly during sex.
Only 40 of the 200 HPV strains target the cervix, but often the body clears the virus naturally.
2) Sexually transmitted infections (STIs) like chlamydia can create an environment for HPV to thrive.
Regular check-ups are crucial, especially for those sexually active outside monogamous relationships, as some STIs often have no symptoms.
3) Sexual history -Women with multiple partners or who are sexually active before 18 are more at risk due to increased exposure to HPV.
4) Smoking increases cervical cancer risk. It allows cancer-causing chemicals to enter the bloodstream and travel throughout the body.
5) Long-term use of oral contraception may increase cervical cancer risk, but the risk reduces after stopping.

6) Multiple pregnancies might elevate HPV infection risk due to increased sexual activity and potential immune system weakening during pregnancy.
Hormonal changes during pregnancy could also make women more vulnerable to HPV and cancer growth.
7) Genetic factors might make some women more susceptible to HPV due to their inherited bodies' inability to fight it.
What are the Early Signs of Cervical Cancer?
Cervical cancer rarely has any symptoms in its initial stages. If symptoms do occur here are the early signs:
- Vaginal bleeding after sex
- Periods that are heavier or last longer than usual
- Watery vaginal discharge that has blood or a strong odour
- Pain during sex
- Vaginal bleeding after menopause
Advanced cervical cancer may include the symptoms mentioned above plus:
- Blood in urine and/or pain during urination
- Bleeding from the rectum and painful or difficult bowel movements
- Swollen legs
- Dull backache
- Abdominal pain
How to Prevent Cancer of the Cervix
a) Cervical Cancer Screening
Regular screening is one of the best ways of detecting cervical cancer early. Pap smears are recommended every 3 years for women aged 21 to 65 years. Additionally, a patient can undergo a co-test (Pap + HPV) every 5 years.

b) HPV Vaccine
The HPV vaccine is designed to protect against certain cancers caused by the human papillomavirus. It prevents infections that can lead to cancers of the cervical, anal, throat, vaginal, vulva and penile
The best time for the vaccine is before someone becomes sexually active. Both men and women can get the HPV vaccine. However, the vaccine can only protect you from HPV strains you have not encountered before.
The age recommendations for getting the vaccine are:
- Children between ages 11 to 12 years
- Young adults up to and including 26 years
- Some adults up to and including 45 years
You should receive recommendations from your healthcare provider on the suitability of getting the HPV vaccine.
FIGO Stages Of Cervical Cancer
The stages of cervical cancer are classified according to the International Federation of Gynaecology and Obstetrics, FIGO system.
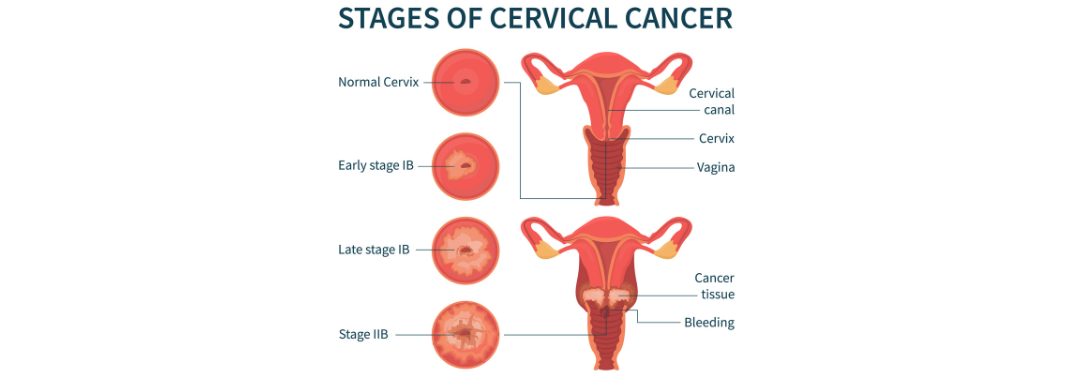
The 3 main cervical cancer stage indicators include:
a) How far the cancer has spread within the cervix
b) If it has spread to nearby tissue or lymph nodes (contain white blood cells that help the body fight diseases and infections)
c) If the cancer cells have migrated from the original tumour to the lymph nodes or other organs
Stage 1
In its earliest stages, the cancer is confined to the cervix and hasn't spread. This stage can be further categorised based on the size of the tumour:
1A: The cancer is very small, only detectable through a microscope.
1B: The tumour is larger but still limited to the cervix:
1B1: Tumour size is 2 cm or less but deeper than 5 mm within the cervix.
1B2: Tumour size is between 2 cm and 4 cm.
1B3: Tumour size is at least 4 cm.
Stage 2
The cancer hasn't spread far. It's localised to the upper vagina, or the tissues surrounding the uterus and hasn't reached the lymph nodes or other parts of the body.
This stage is divided based on the extent of spread:
2A: The cancer has reached the upper part of the vagina, but not the surrounding tissues. This stage can be further categorised by tumour size:
2A1: The tumour is 4 cm or smaller.
2A2: The tumour is larger than 4 cm.
2B: The cancer has spread to the tissues around the uterus (parametrium).
Stage 3
The cancer has progressed to the lower vagina and potentially the surrounding pelvic tissues.
At this stage the tumour size may be impacting kidney function by potentially obstructing the tubes responsible for transporting urine. It's also possible the cancer has spread to nearby lymph nodes.
3A: The cancer is confined to the lower part of the vagina without involving the pelvic walls.
3B: The cancer has spread to the pelvic walls or is causing problems by blocking the ureters.
3C: The cancer has reached nearby lymph nodes. This stage is further divided based on the location of the affected lymph nodes:
3C1: Lymph nodes within the pelvis are involved.
3C2: Lymph nodes near the major artery (aorta) are affected.
Stage 4
The cancer may have spread to nearby organs like the bladder or rectum, or even beyond the pelvic area to other parts of the body.
4A: This indicates the cancer has grown into nearby organs or is starting to spread outside the pelvis.
4B: This signifies a more advanced spread, where the cancer has reached distant organs like the liver, lungs, bones, or lymph nodes.
Need a cervical cancer diagnosis? Get in touch with an oncologist today!
What Are the Available Treatment Options for Cancer of the Cervix?
Following a cervical cancer diagnosis, a gynaecologic oncologist leads creates a personalised treatment plan for a patient based on a thorough evaluation.
1) Surgery
The type of surgery recommended will depend on the extent of your cancer. Early-stage cancers may be treated with a conisation, which removes a cone-shaped piece of tissue from the cervix.

In some cases, a trachelectomy may be possible, preserving the uterus and ovaries while removing the cervix and upper vagina.
For more advanced stages, a radical hysterectomy might be necessary, removing the uterus, cervix, upper vagina, and surrounding lymph nodes. In rare situations, a more extensive surgery called a pelvic exenteration might be needed.
Benefits: Surgery offers the potential for complete removal of the cancer, potentially leading to a cure in early stages. Additionally, some surgical options may allow for preserving fertility.
Considerations: Recovery time and potential side effects like pain, bleeding, and infection vary depending on the surgery. Fertility may also be impacted depending on the type of surgery performed.
2) Chemotherapy
Chemotherapy uses powerful drugs delivered intravenously (through a vein) or sometimes orally (in pill form) to kill cancer cells throughout the body.
It can be used in different ways:
i) Adjuvant therapy: Given after surgery to reduce the risk of cancer recurrence in high-risk cases.
ii) Concurrent therapy: Combined with radiation therapy to improve treatment effectiveness for locally advanced stages.
iii) Palliative care: Used to manage symptoms and improve quality of life in advanced stages.
Benefits: Chemotherapy significantly increases the chances of successful treatment, especially when combined with other therapies.
Considerations: Chemotherapy can cause side effects like nausea, fatigue, hair loss, and increased risk of infection. It's crucial to discuss these side effects with your doctor and explore supportive care options to manage them.

3) Brachytherapy
Brachytherapy is a form of internal radiation therapy where radioactive material is placed close to the tumour site within the vagina or cervix.
There are two main types:
a) High-dose-rate (HDR) brachytherapy: A temporary placement of radioactive implant for a short period.
b) Low-dose-rate (LDR) brachytherapy: A temporary placement of radioactive seeds for several days.
Benefits: Brachytherapy delivers a high dose of radiation directly to the tumour while minimising exposure to surrounding tissues. This can be beneficial for certain cases.
Considerations: Brachytherapy may cause temporary side effects like vaginal discomfort, bleeding, and urinary problems.
4) Radiation Therapy
Radiation therapy uses high-energy X-rays or other forms of radiation to destroy cancer cells.
External beam radiation therapy (EBRT) uses a machine outside the body to direct radiation beams towards the cancer area.
Radiation therapy can be used in various ways:
i) Primary treatment: For early-stage cancers, especially when surgery is not ideal.
ii) Concurrent therapy: Combined with chemotherapy for locally advanced stages.
iii) Adjuvant therapy: After surgery to reduce the risk of recurrence.
iv) Palliative care: To manage symptoms and improve quality of life in advanced stages.
Benefits: Radiation therapy is effective in destroying cancer cells and can be used for curative purposes or to manage symptoms.
Considerations: Radiation therapy may cause side effects like fatigue, skin irritation, and temporary bowel or urinary changes. These are typically manageable with proper care.
5) Proton Therapy
Proton therapy is a newer and more precise form of radiation therapy that uses protons (particles) instead of X-rays.
Benefits: Proton therapy offers increased accuracy in targeting cancer cells, potentially reducing damage to surrounding healthy tissues. This can be beneficial for tumours close to critical organs or for patients who have already received radiation therapy.
Considerations: Proton therapy is available at Apollo Cancer Centre. Discuss with your doctor to see if it's a suitable option for you.

6) Immunotherapy
Immunotherapy is a type of treatment that helps your body's immune system recognise and attack cancer cells. There are two main approaches to immunotherapy:
Checkpoint inhibitors: These drugs help remove "brakes" on the immune system, allowing it to better target cancer cells.
Factors that determine cervical cancer treatment options include:
- Stage of cervical cancer
- Age of the patient
- Available treatment options
- Personal preferences
- Medical history

Best Cervical Cancer Treatment Hospitals
Here's a look at some hospitals worldwide that offer advanced cervical cancer treatment and a supportive environment.
Thailand
Bumrungrad International Hospital: JCI-accredited Bumrungrad provides a full spectrum of cancer treatments, including minimally invasive surgery and targeted therapies.
India
Apollo Cancer Treatment Centre: Stands out for its cutting-edge technology, including proton therapy treatment for cervical cancer.
MIOT International Hospital: MIOT brings together specialists in oncology, surgery, and radiation therapy to create optimal treatment plans.
Max Healthcare: Offers comprehensive care, from early detection to advanced cervical cancer surgical procedures.
Wockhardt Hospitals: Wockhardt leverages advanced diagnostics and a team of experienced oncologists for personalised treatment plans.
Turkey
Anadolu Medical Centre: Anadolu offers a dedicated oncology department with advanced technology and a patient-centric approach.
Acibadem Group of Hospitals: This prestigious group features a network of facilities with highly skilled doctors and access to the latest treatments.
Medipol Hospital: Known for its integrated approach, Medipol offers surgery, radiation therapy, and innovative therapies like immunotherapy.
Liv Hospital: Liv prioritises patient comfort alongside cutting-edge treatments, fostering a supportive environment for healing.
Singapore
Raffles Hospital: Offers comprehensive care, from screening and diagnosis to advanced surgical and radiation therapy options.
Tanzania
Aga Khan Hospital, Dar es Salaam: This renowned hospital provides a high standard of care for cancer patients, including those with cervical cancer.
Kenya
HCG CCK Cancer Centre: This specialised centre offers comprehensive care for various cancers, including cervical cancer.
AAR: Oncology expertise complimented with advanced cancer diagnostic and surgical equipment.
Nairobi West Hospital: Nairobi West Hospital offers oncology services, including treatment for cervical cancer.
United Kingdom
The London Clinic Hospital: This prestigious hospital provides advanced treatment options and personalised care for cervical cancer.
United Arab Emirates (UAE)
Saudi German Hospital - Dubai: This JCI-accredited hospital offers a multidisciplinary approach to cervical cancer care.
NMC Hospital - Abu Dhabi: NMC utilises advanced technology and a team of experienced oncologists for effective cervical cancer treatment.
King's College Hospital - Dubai: Offers specialised cervical oncology services.
American Hospital - Dubai: This American-standard hospital provides advanced cancer care, including treatment for cervical cancer.